- May 17, 2019
- Posted by: info
- Categories: Biomechanics, Research
Background
Arterial stiffness is recognized as a predictive indicator of vascular disease [1,2] and then, used in both diagnosis and treatment planning. Several arterial stiffness definitions – based on in vivo measurements – have been proposed in the literature [3-5]. Experimental studies have evidenced regional variations in the stiffness of the aortic district [6-7]. Consequently, measures localized of pressure and diameter can be poor for a proper mechanical characterization.
Goal
The goal of the present research activity is to develop a semi-automatic method to assesses dimension and shape of descending aorta from non-contrast CT data sets. Such computed geometrical information are used to evaluate the aortic stiffness and its changes along the length of the investigated district.
Methods and results
The adopted method is developed in the following three stages: 1. Analysis of medical image; 2. Non-invasive measures of cross-section area/diameter; 3. Computation of aortic stiffness parameters.
1. Analysis of medical image.
Medical image analysis aims at the reconstruction of a three-dimensional model of the descending aorta and to get information on the three-dimensional deformation of such a district during the cardiac cycle. The medical images used in the present study are a collection of DICOM files corresponding to 20 time instants of the cardiac cycle (from 0% to 95% of RR-time interval). The reconstruction of three-dimensional model of is performed through a process of semiautomatic segmentation using the open source software ITK-Snap (www.itksnap.org). Figure 1 shows the main interface of the software with the axial and sagittal (DICOM) images as well as the coronal reconstructions of the descending aorta.
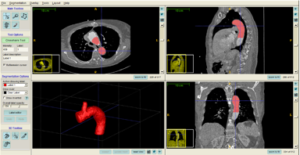
Figure 1. Interface of software ITK-Snap. Viewing of DICOM images and segmented 3D model of descending aorta.
2. Non-invasive measures of cross-section area and diameter.
Eight cross-sections are detected along the descending aortic district. For each section, the cross-section area and the corresponding diameter are computed. Assuming data repeatability, the waveform of cross-section area is created, defining the trend of area/diameter data during the cardiac cycle.
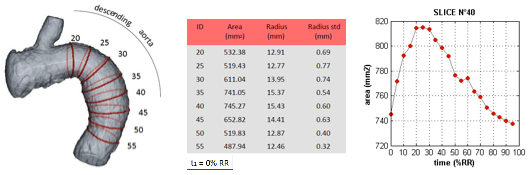
Figure 2. Detection of cross-section area along the descending aorta district and construction of area-data waveform defined between two consecutive minimum of the cardiac cycle.
3. Computations of aorta stiffness parameters.
Aortic stiffness is calculated, for example, through the Peterson modulus and Young modulus [6,7], whose definition involves the knowledge of (relative and/or absolute) changes in blood pressure and luminal cross-sectional area (diameter). Such differences are evaluated between the maximum and minimum values reached during the cardiac cycle (points at the end of systole and diastole).
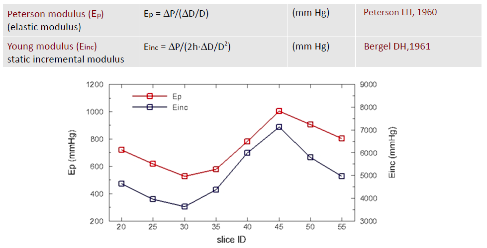
Figure 3. Variation of Peterson modulus (Ep) and Young modulus (Einc) along the descending aorta district.
References
- K. Cheng, C. R. Baker, G. Hamilton, A. P. G. Hoeks, S. A. M., Arterial elastic properties and cardiovascular risk/event, European Journal of Vascular and Endovascular Surgery 24 (2002) 383397.
- U. Quinn, L. A. Tomlinson, J. R. Cockcroft, Arterial stiffness, Journal of the Royal Society of Medicine Cardiovascular Disease 1 (2012) 1–18.
- M. F. O’ourke, J. A. Staessen, C. Vlachopoulos, D. Duprez, G. E. Plante, Clinical applications of arterial stiffness; definitions and reference values, American Journal of Hypertension 15 (2002) 426–444.
- J. J. Oliver, D. J. Webb, Noninvasive assessment of arterial stiffness and risk of atherosclerotic events, Arteriosclerosis, Thrombosis, and Vascular Biology 23 (2003) 554–566.
- S. Laurent, J. Cockcroft, L. Van Bortel, P. Boutouyrie, C. Giannattasio, D. Hayoz, C. Pannier, B.and Vlachopoulos, I. Wilkinson, H. Struijker-Boudier, Expert consensus document on arterial stiffness: methodological issues and clinical applications, European Heart Journal 27 (2006) 2588-2605.
- J. Kim, J-W. Hong, S. Baek, Longitudinal differences in the mechanical properties of the thoracic aorta depend on circumferential regions, Journal of Biomedical Materials Research Part A (2012).
- L.H. Peterson, R.E. Jensen, J. Parnell, Mechanical properties of arteries in vivo, Circulation Research (1960); 8:622–639.
Acknowledgements
- Cariplo Foundation through the AVAS_PRO project.

